All about Actinic keratosis
Actinic keratosis is an area of the skin damaged by ultraviolet radiation that appears in zones exposed to the sun for years. Its appearance is variable.
What is actinic keratosis?
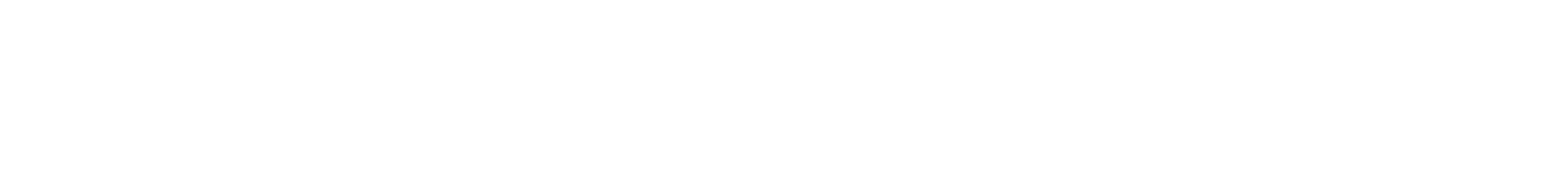
Actinic keratosis or solar keratosis is an area of sun-damaged skin occurring mostly in zones that are chronically exposed to ultraviolet (UV) radiation. It is usually found on the face, ears, lips, bald scalp, forearms, dorsa of the hands and lower legs.
Actinic keratoses can grow to a centimeter or two in diameter. Although at first, they may be difficult to see, they are easily distinguished because they are usually rough and scaly areas. Their appearance is variable. In fact, the same person can have different actinic keratoses with a different color, thickness and extension.
Risk factors: actinic keratosis and sun exposure
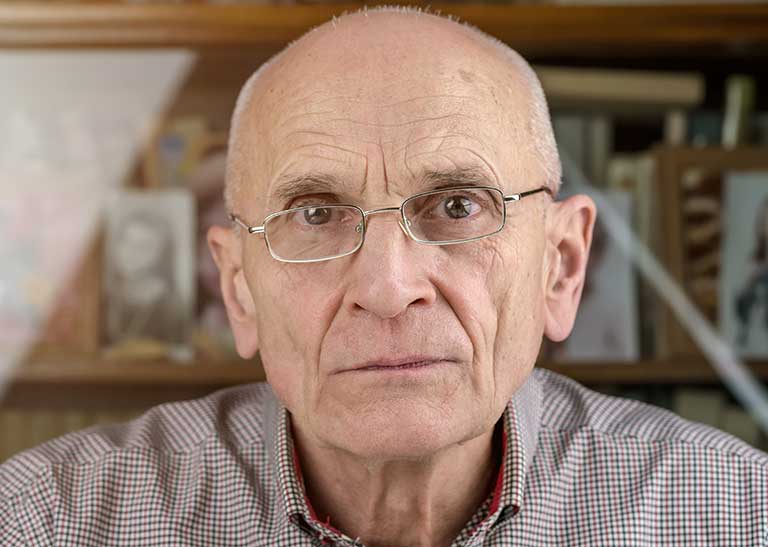
Exposure to accumulated UV radiation over to many years is mostly responsible for the development of actinic keratosis hence, why it occurs most commonly in older people. This accumulation results from sunbathing, from using tanning beds or from working or playing sports outdoors.
It is true that, while sunbathing affords certain beneficial effects—for instance, sunlight is necessary for the skin to produce vitamin D—excessive exposure to UV light causes mutations in the DNA of skin cells. This favors premature photoaging and the development of actinic keratosis and skin cancer.
What are the symptoms of actinic keratosis and how is it diagnosed?
Actinic keratosis usually occurs in adults with fair skin in the form of rough, scaly spots, plaques or lumps. These spots can vary in color, can present as single or multiple lesions, and appear on sun-exposed areas. The surrounding skin may also be affected and look a different color or present small broken blood vessels. Even if it looks normal, this surrounding skin which is called field of cancerization can present alterations that can only be seen under a microscope.
Although actinic keratoses does not usually give any symptoms, they can sometimes cause itching or bleeding. You should always check with your doctor if you notice any of these symptoms.
Usually, the doctor will only need to examine the lesions to be able to diagnose actinic keratosis. Only when in doubt, the doctor will do a biopsy, which involves removing and sending off a sample of the lesion for microscopic examination in the laboratory.
References
- De Berker D, Mcgregor JM, Mohd Mustapa MF, Exton LS, Hughes BR. British Association of Dermatologists’ guidelines for the care of patients with actinic keratosis 2017. Br J Dermatol [Internet]. 2017 [cited 2020 Feb 19]; 176(1):20-43. Available at: https://onlinelibrary.wiley.com/doi/full/10.1111/bjd.15107
- BAD: British Association of Dermatologists. Actinic Keratoses - Also Known as Solar Keratoses [Internet]. London (United Kingdom): BAD; 2007 May [revised 2019 Nov; cited 2020 Feb 19]. 5 p. Available at: http://www.bad.org.uk/shared/get-file.ashx?id=66&itemtype=document
- Berman B, Cockerell CJ, Zografos P. Pathobiology of actinic keratosis: Ultravioletdependent keratinocyte proliferation. J Am Acad Dermatol [Internet]. 2013 Jan 1 [cited 2020 Feb 19];68(1 Suppl.1):S10–9. Available at: https://www.jaad.org/article/S0190-9622(12)01065-1/fulltext
- Moy RL. Clinical presentation of actinic keratoses and squamous cell carcinoma. J Am Acad Dermatol [Internet]. 2000 Jan [cited 2020 Feb 20];42(1 Suppl. 1):S8–10. Available at: https://www.jaad.org/article/S0190-9622(00)27494-X/fulltext
- Werner RN, Stockfleth E, Connolly SM, et al. Evidence- and consensus-based (S3) Guidelines for the Treatment of Actinic Keratosis - International League of Dermatological Societies in cooperation with the European Dermatology Forum – Short version [Internet]. J Eur Acad Dermatol Venereol. 2015;29(11):2069-79. Available at: http://doi.wiley.com/10.1111/jdv.13180
- Gohara M, Morison W, Sarnoff DS. Clothing: Our first line of defense [cited 2020 Feb 6]. Inn: The Skin Cancer Foundation [Internet]. New York (USA): The Skin Cancer Foundation; c2019. - [approx. 5 screens]. Available at: https://www.skincancer.org/skin-cancer-prevention/sun-protection/
Frequently asked questions about actinic keratosis
Actinic keratosis is not hereditary, although some of the factors that favor its appearance, such as fair skin or freckles, are so. Actinic keratosis is not contagious.
Actinic keratosis is an uncontrolled proliferation of keratinocytes: the most abundant cells of the epidermis (the outermost layer of the skin), that become abnormal4. Some actinic keratoses can turn into a type of skin cancer called epidermoid carcinoma or invasive squamous cell carcinoma1,4. Although rare, this type of cancer can spread to other tissues, and it is therefore recommended to treat all actinic keratoses.
Furthermore, a person with actinic keratosis is at higher risk of developing any type of skin cancer compared to another person of the same age who does not. People who have a higher number of actinic keratoses also run a higher risk of skin cancer.
Some actinic keratoses resolve spontaneously, especially if sunscreen or protection is used, although most remain as they are. Others may progress into invasive squamous cell carcinoma. Unfortunately, it is impossible to know in advance which ones will in fact progress into invasive squamous cell carcinoma. The clinical course of the condition cannot be predicted.
Actinic keratosis lesions can heal and disappear spontaneously or through treatment. However, it is very common for old lesions to recur or for new ones to come out. The presence of a single actinic keratosis is already a sign that chronic damage from solar radiation has occurred, and hence there is a risk that other lesions could appear. Therefore, if you have actinic keratosis, your doctor will monitor you regularly, and will recommend that you seek consultation if you notice new lesions or any changes in the ones you already have.
Protecting yourself from the sun is essential to prevent the appearance of actinic keratosis and slow down progression. Following the following measures strictly is key to keeping actinic keratoses under control:
Use sunscreen and clothing that covers your body.
- Avoid peak sun hours.
- Avoid artificial sunlight (sun beds/tanning salons).
- Check your skin at home and schedule an appointment with the dermatologist on a regular basis.
